
The state of Missouri is removing an unprecedented number of people from its Medicaid program, possibly leaving as many as 220,000 residents, including almost half of them children, without health insurance. This loss, occurring between June 2023 and January of 2024, is attributed to the “unwinding period,” a 12-month process of reversing public-health emergency (PHE) policies that had automatically renewed Medicaid coverage. Three quarters of those who lost their insurance were deemed ineligible for procedural reasons, meaning they were kicked out of the program due to issues like missing paperwork, not because they no longer qualify. The unwinding is only two-thirds complete, and more must be done to ensure all those who are still eligible keep their health coverage.
Under federal rule during the PHE, states agreed to suspend the regular process of periodically redetermining Medicaid enrollees’ eligibility in exchange for additional federal dollars. Three years after the onset of the COVID-19 pandemic, Missouri resumed the regular redetermination process for all beneficiaries on June 1, 2023, with all reviews to be completed by the end of May. This will ultimately impact more than 1.5 million MO HealthNet beneficiaries – almost a quarter of the state’s population.
Any loss or gap in coverage can be dire for those who must choose between receiving essential health care and affording other necessities. For Missourians who are most at risk of poor health outcomes, specifically older adults, people with disabilities, and low-income adults and children, the consequences could be catastrophic.
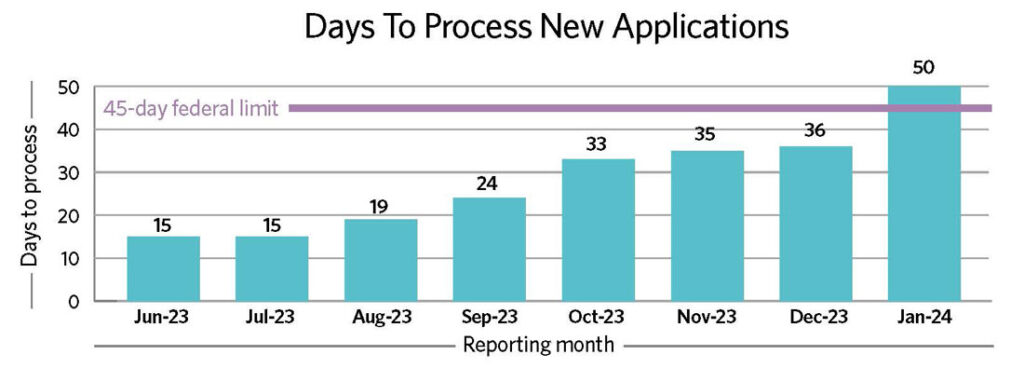
For those who have to reapply after losing coverage, delays in processing new applications are getting worse by the month. Applicants are waiting an average of 50 days for a determination, putting Missouri out of compliance with the federal 45-day limit. This figure has been trending upward since the start of the unwinding and rose by almost 40% between December and January, posing a serious concern for almost 65,000 Missourians waiting for coverage.
The situation is alarming, but there are ways to ease challenges for enrollees as well as state agencies that are struggling to keep up with the growing backlog. As we look to the next several months and hundreds of thousands of Missourians still to be reviewed, there are realistic policy solutions that could be implemented to make this process more accurate. Learn more in our one-page fact sheet and our latest brief, Missouri Medicaid Unwinding Post-Public Health Emergency.


