
Medicaid is a safety net insurance program that allows Missourians to see a doctor when they are sick, get checkups, buy medications, and go to the hospital. Having health insurance allows people to maintain their health, go to work, and take care of their families. The Medicaid program, however, is intricate, with many different pieces and rules that can be tough to navigate.
This complexity is exactly why MFH releases an annual publication, Missouri Medicaid Basics, that unpacks the various moving parts of the program. While preparing this year’s version, a few things stood out to me as key takeaways that Missourians should know about our Medicaid program, MO HealthNet.
First, eligibility levels for most groups are surprisingly low, especially for parents – who qualify for the program only if they make less than 22% of the federal poverty level. That is about $5,500 per year for a family of four. Also, under current law, adults without children don’t qualify for the program at all, no matter how little they make. That means that many Missourians fall into the coverage gap, making too much to qualify for Medicaid but too little to qualify for subsidized private insurance. Fortunately, Medicaid expansion was approved by ballot initiative in August of this year. Once it is implemented in July of 2021, parents and childless adults will be able to participate in the program if they make less than 138% of the federal poverty level, ensuring that many more Missourians have a path to health care access.
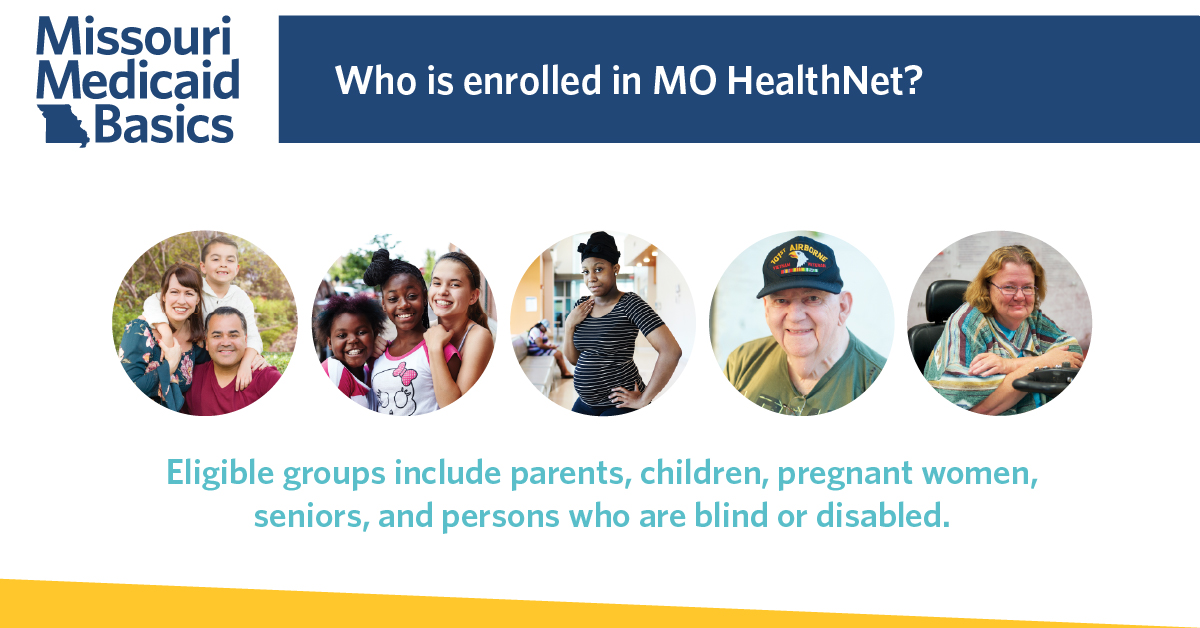
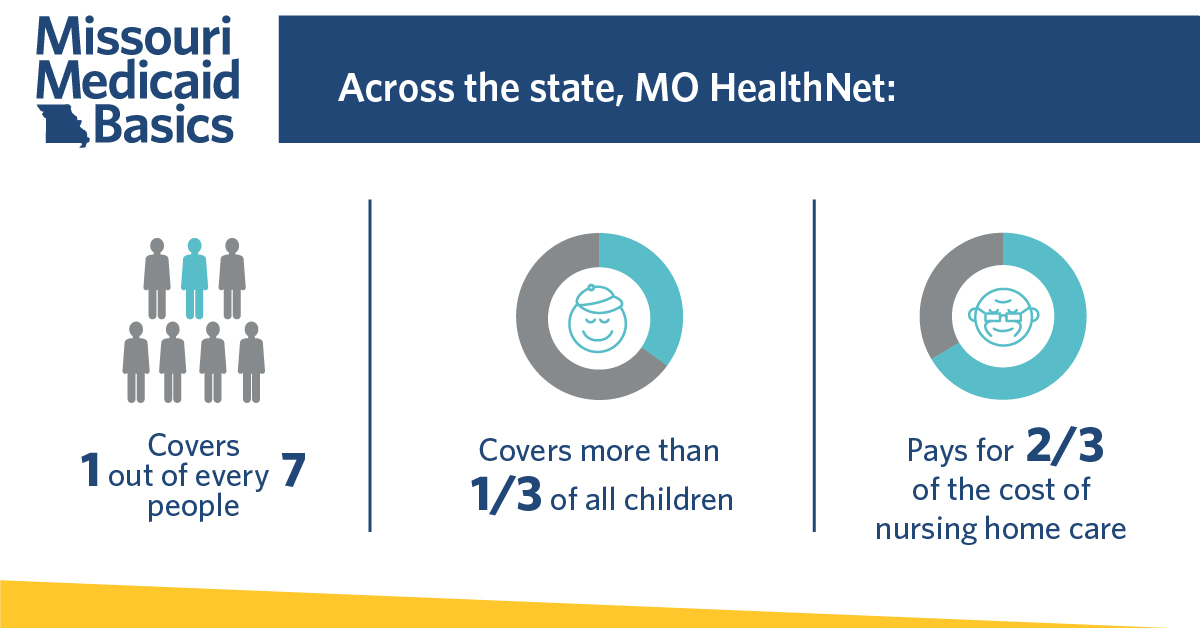
Second, MO HealthNet offers coverage to many different groups of people. From seniors and disabled populations to children and pregnant women, the program allows low-income Missourians from all walks of life to access health care. This also means that the program is complex, with different sub-programs for each eligibility group. This complexity makes it difficult to paint the program with broad strokes, as the delivery and eligibility criteria are tailored to various types of participants.
Lastly, during times of emergency, the Medicaid program can adapt to ensure coverage for Missourians in need, which has been highlighted during the current COVID-19 pandemic. With the relaxing of certain requirements, copays for COVID-19 testing and treatment have been waived, and access to virtual care through telehealth is easier than ever. During a time of crisis, Medicaid makes health care more accessible, giving Missourians peace of mind and ensuring the health of communities.
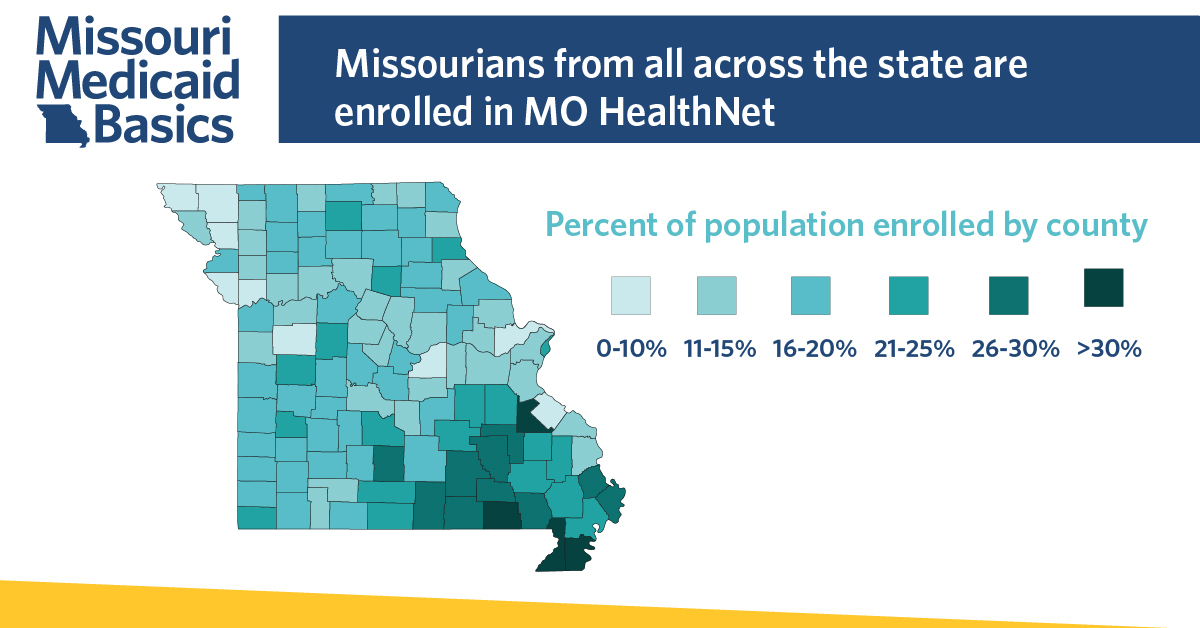
Across the country, and especially in Missouri, the Medicaid program has received more attention than ever. With the recent passage of Medicaid expansion in Missouri and other states, the COVID-19 pandemic’s impact on the health and economic stability of the nation, and the pending Supreme Court case that could overturn parts or all of the Affordable Care Act, it has never been more imperative to recognize the scale, scope, and complexity of the Medicaid program.
Reading our full Missouri Medicaid Basics publication, or even viewing our At-a-Glance factsheet, will give you new appreciation and perspective about this important component of the safety net. In order for us to streamline and strengthen MO HealthNet moving forward, we must start with a firm basic understanding of the many pieces that make up this essential program.


